Congenital Adrenal Hyperplasia is one of the most common medical terms associated with intersex genital differences. A mom and nurse sits down with an intersex advocate to uncover common misconceptions around genital surgery.
By Hans Lindahl and Stephani Lohman
ALSO AVAILABLE IN SPANISH! “Una mamá y enfermera desmiente 5 mitos sobre la cirugía genital y la Hiperplasia Suprarrenal Congénita. Entrevista a Stephani Lohman por Hans Lindahl” Thank you to Laura Inter of Brújula Intersexual for offering translation!
Stephani is a registered nurse working in Milwaukee, Wisconsin. She has years of experience doing research and self-advocating for her child with CAH. Stephani and her partner, interACT Board member and University of Wisconsin professor Eric Lohman, co-authored a book called Raising Rosie: Our story of Parenting an Intersex Child. *Note that the child mentioned in Stephani’s book has since grown up and transitioned, and so we refer to him with his present name, Wade, and he/him pronouns moving forward.*
Hans is an intersex person with over 5 years of leadership experience in intersex media and legislative work. Their work includes helping youth with CAH tell their own stories. They are also a member of interACT Youth, a youth group that brings together young advocates across many different medical diagnosis terms, including CAH.
Frequently Asked Questions About Genital Surgery for Congenital Adrenal Hyperplasia

Stephani hugs Wade, her son, who is a transgender boy with Congenital Adrenal Hyperplasia.
Hans: What was your experience being the parent of a child with Congenital Adrenal Hyperplasia, and navigating genital surgery?
Stephani: I had noticed right away that my baby’s genitals did not look like what any of my other children had. A couple days later, a urologist suggested that we do elective surgery: a clitoroplasty [surgery to reduce the size of a clitoris], and a vaginoplasty [surgery to create or increase the size of a vagina] to make our baby look more “typically female.”
We argued back, saying that we had done a little research on our own and it didn’t seem like this was a good suggestion. It didn’t seem like he gave us all the options, including waiting and doing nothing. That led us into a pretty contentious relationship that went on for about a year, where this doctor continued to suggest that we perform surgery to “normalize” our baby’s genitals.
We decided that we would wait and let our child make an informed choice on their own, since it is their body. Ultimately we parted ways with the urologist because we had a fundamental disagreement.
Hans: I think that the two of you were especially well-positioned to ask the questions that you did about Congenital Adrenal Hyperplasia and genital surgery, because you’re a nurse and Eric is a college professor.
There’s a lot of misinformation out there. I think all parents want the best for their children and would find it hard to imagine that doctors might ever advocate an option that … might not be that.
Stephani: I think that it’s hard to imagine that doctors are not the authority on everything. They may believe genital differences cause social problems, but that has never been shown, and urologists are not the authority on psychology. Doctors like our urologist probably think that they’re coming from a place of honesty, and looking out for children.
It’s very important for parents to know that you have the right to ask questions. You can ask, “How do you know this? Can you show me the evidence? And is there a standard of care that you’re following or why are you recommending this?” Most importantly: “What happens if I do nothing?“
Usually they’ll give you an answer like, “well, you might have a child who suffers from many UTIs.” And you can say, “Well, how do you know that?” In reality, there is evidence that genital surgery can actually increase the risk a child will have UTIs,[1] but you might have to have some medical knowledge to dig for studies in order to ask those questions.
Asking questions is hard. But the decisions that you’re making for your child surgically are forever. People can always choose surgery for themselves later on, but you can never get back what has been removed, so it’s very important to be thoughtful about that. In our case, our child ended up growing up to express a male gender identity. 5-15% of all kids born with genital differences connected to Congenital Adrenal Hyperplasia end up not being female.[2] And even for those who do grow up to have a female gender identity, how can we be certain they might not want to grow up with their original bodies, or decide based on how they feel later?
Surgery and “Ambiguous Genitalia”
Hans: A lot of infants with CAH are born with what are sometimes considered intersex genitalia, or the outdated term, “ambiguous genitialia.” In addition, CAH does come with some very serious hormonal concerns. However, addressing the very real hormonal issues is NOT related at all to decisions about genital surgery.
Stephani: Yes. Genital surgery or not, the underlying medical condition will still persist for life.
When a fetus with CAH is in utero, they are exposed to extra testosterone. So for a fetus that is headed toward developing a penis anyway, the body is typically going to respond that way to testosterone already. But in a fetus that was typically going to develop a vulva and clitoris, that extra testosterone can cause what we might call genital differences. Because these unexpected differences are visible right at birth, some parents may feel confused and distressed, leading doctors to think of genital differences as social emergencies.
Some doctors might talk about genital surgery for CAH as “fixing” or “putting a body back” to the way that nature or God intended. But your child’s body already is the way that nature intended it to be. This kind of diversity occurs throughout nature.
Clitoroplasty, or Clitoral “Reduction” or “Repositioning” Surgery
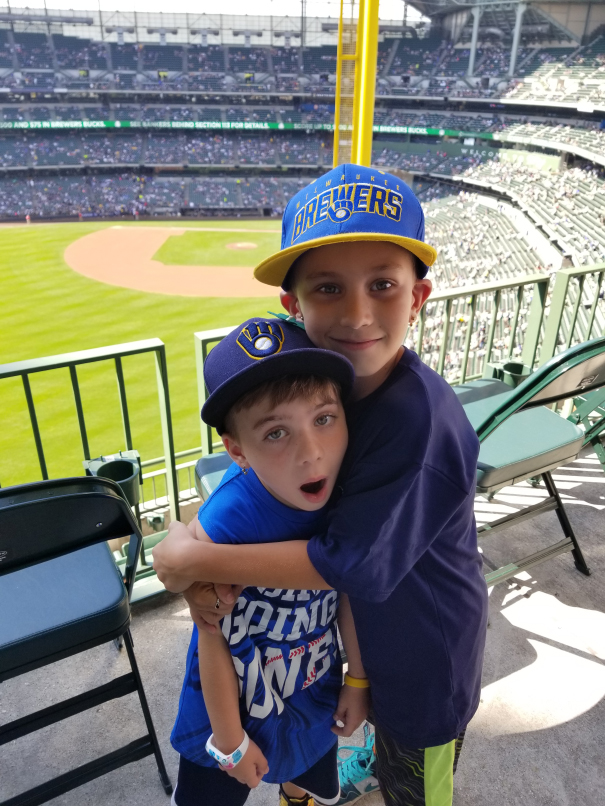
Wade’s older brother hugs him at a family outing to a baseball game.
Hans: Most external genital surgeries are frankly for aesthetic reasons, right? So with surgery decisions, you’re weighing considerations that are subjective and cosmetic against serious long-term risks to sexual and urinary function. It’s not truthful to say that anything can be completely nerve-sparing, or that anything can completely avoid affecting the clitoris.
Stephani: Right. A clitoris is ultimately erectile tissue. Erection of the clitoris or penis happens because there are sacs that fill up with blood, like water balloons. The walls of the sacs themselves are full of nerves that control sensitivity, so when you cut them out to make the clitoris smaller, you are removing many important nerves.
The idea that you are somehow going to be able to spare nerves that are important for sexual function is very short-sighted. Surgery may try to spare the main nerve in the clitoris, but all those many nerves in the erectile tissue will be cut out. There’s no way to avoid it.
Hans: I’ve heard a lot of new terms recently. Doctors might say they’re going to change the way that the clitoris “points” or they’re going to “reposition it.” But it’s definitely unclear what these terms really mean, as far as surgical technique and how parents could understand what’s actually being done.
Stephani: Like any surgery, the average person will have no idea what surgeons are actually doing.
Imagine you were considering a tonsillectomy. You think, “Oh, what is that? Well, taking out your tonsils.” Yes, but how? What are you doing? Are you going in there with a scalpel? Are you grabbing it with some kind of tweezers? All of these things are done miles above the people who are offering consent. Because what the patient wants to know is: am I going to survive? How much pain am I going to be in? What is the recovery like?
So when you are making these decisions, you are thinking about them in the very real moment that you’re in right now: “I get sore throats a lot, I’m going to have this surgery to fix that, and I don’t care how you do it.”
Imagine if a doctor described your tonsillectomy in real terms: “we’re going to go in, and we’re going to shove a tube in your throat with a metal blade, so you’re probably going to be very sore. Your throat is going to hurt, because of the tube. We’re going to put an anesthetic in your lungs. It’s going to make you feel like real crap for a couple days. And while we’re in there, we’re going to use a really sharp scalpel to scoop out some tissue.”
Nobody would do that; right? That sounds terrible. But that’s what is going on. So if surgeons answered questions in this way, nobody would rush to have surgery, especially one that isn’t immediately necessary.
It’s usually not explained to parents how important erectile tissue is for sexual function of both the penis and the clitoris. When nerves are removed with erectile tissue, scarring can be obvious on the outside, cause pain, and interfere with orgasm.
If doctors were honest with parents and explained that surgery carries a risk of pain in future intimate relationships, how would that affect families’ decisions?
Urogenital Sinus Surgery for Congenital Adrenal Hyperplasia
Hans: What is the term “urogenital sinus” I keep hearing about?
Stephani: Children with CAH may have what is called a urogenital sinus, where the urethra and vagina connect inside the body. This means that there is only one opening for fluids to leave the body. Most children with CAH and genital differences have a urogenital sinus with a low confluence, meaning that the urethra connects with the vagina at a point that is close to the outside of the body instead of higher up toward the bladder. Surgery is usually not immediately necessary.
Some doctors tell families that leaving a urogenital sinus alone causes increased risk of urinary tract infections (UTIs), but this is false and misleading. In fact, children who do not have surgery for a urogenital sinus have no greater risk of UTIs than those who do. It is actually the opposite—it’s been shown that surgery itself can increase UTI risk.[1]
Surgery can also cause incontinence, or leakage of urine. For most people, urine does not dribble out on its own. The urine stays in your bladder because you have a sphincter: it opens, you urinate, it closes, and you’re done. Some people will be incontinent because of surgery if the sphincter or the nerves that control it are damaged.
Surgery for Congenital Adrenal Hyperplasia and UTIs
Hans: So the idea that genital surgery protects against UTI risk is wrong?
Stephani: Yes. Urologists may quickly promote surgery, but surgery can actually increase the chance that your child will get UTIs. Think about it: you opened a sterile region of someone’s body, cut tissue, and moved things around. This creates scar tissue that can interfere with urinary function. Afterwards, it makes sense that we’d see UTIs increase. And we know that kids with a urogenital sinus and CAH don’t get more UTIs if they don’t have surgery.
I think a lot of the urologists get ideas from their older teachers, and they can honestly believe these things to be true. They believe that UTIs might be caused by CAH, instead of the surgery itself. They believe that they’re doing a service for these parents.
Vaginal Surgery and Menstruation
Hans: I know the surgeries done for urogenital sinus basically involve making a separate opening for the vagina. So suppose that a family decided to opt for the vaginal surgery that was recommended because of UTI risk, or urine pooling, or anything else families are commonly told… those vaginal surgeries are serious and can take multiple followup operations.
Stephani: Yes, surgery to separate the vagina and reposition it to open on the outside during urogenital sinus surgery is often recommended. But a baby has no need for a vagina, and scar tissue from surgery can narrow or close off the vagina. This means more surgery may be needed at puberty to open that blockage so blood can come out.
Parents may think there will be a perfect little vagina… really, there is going to be a lot of scar tissue. Anytime you cut, it makes a scar. And scar tissue can also cause difficult or painful sexual intercourse. The idea that you need to construct a vaginal opening or repair a urogenital sinus for an infant is not supported by medical literature.
Hans: Is surgery necessary for menstrual blood to leave the body?
Stephani: After we rejected infant surgery, one day I went to change my baby’s diaper and saw pink residue. Of course I was thinking incorrectly at the time, “oh, this urogenital sinus must be causing a UTI.”
So I took Wade to the pediatrician, who said, “this looks like uterine blood.” She analyzed the tissue, and it was menstrual blood. Any newborn with a uterus can have this kind of uterine bleeding, because the mom’s hormones might be still circulating.
Hans: So wait… if a child is born with a urogenital sinus, and you do not do surgery, menstruation would naturally come out of the body… through the urogenital sinus?
Stephani: Yes.
Hans: Is there any way in which that could be bad, or require surgery when they are older?
Stephani: If menstrual fluid could not leave the body at all, then surgery would be necessary because you would have pain. As long as your menses can pass through the urethra, then there wouldn’t be any immediate medical need for surgery. The only consideration is that you would not be able to use a tampon or menstrual cup.
There are a lot of pressures doctors face. The medical view of “normal” is usually not representative of the real diversity of human bodies. It’s hard to untie all of the things that come with the culture of a profession.
I don’t think that most parents are given enough information to make a truly informed choice. You need to lay out not just what to expect during and after the surgery, but during and after the surgery for a lifetime. Look: I don’t want to think about my child having sex, but they’re going to do it eventually. Most people do. So do you live with the guilt that you may have doomed your child to painful sex or that you may have made a decision that your child may not support? How will you know?
There should be a protocol, and it should be watchful waiting. It takes so long to move the ship of medicine. If you have new evidence, it takes 10, 15, or even 20 years for it to come to market. The profession is not going to change out of the goodness of its own heart, because most doctors believe that these surgeries are helping people, even though that’s based on discredited assumptions from the 1950’s and studies that have ignored many adult patients’ voices.
Advocating for Your Child with Congenital Adrenal Hyperplasia

Wade smiles big, trying on a goofy fake mustache.
Hans: What advice do you have for parents of children with CAH? How can they best equip themselves to sift through all this information and to advocate for themselves and their child?
Stephani: I would say, reach out. interACT or InterConnect can put you in touch with other parents who are going through the same thing. You can also talk to adults who have been through it and have lived the experience. The more information you have from a variety of sources, the better.
Hans: I will say that what we’re about at interACT is centering individual informed consent. 99% of the time, that’s going to mean waiting on genital surgeries. And that’s what top human rights organizations are saying, that’s what LGBTQ organizations are saying. It’s not a radical position.
Stephani: No. Delaying surgery is not a fringe position. Every person should have the fundamental right to make choices about their own body. That is the key. Sometimes you won’t have that right because you’re in a life-threatening medical situation. But that isn’t the case for most children with CAH. Delay is okay. It’s not an emergency.
And genital difference can be private without being shameful. You can have a private discussion and make a private decision and never tell anybody, but still make your child feel comfortable in their own skin. When Wade reaches an age where he looks back and reflects upon his childhood, I want him to feel I was proud of him, not ashamed, no matter what body he was born in.
Hans: I also want to be clear that I never want to blame parents who may have already chosen surgery. Everyone wants to do what’s best for their child, and it can be really confusing to sift through medical authority and all the misinformation that’s out there. So if there are parents, for example, who did choose surgeries on their CAH kids, my intention is never to shame them or say that they made a wrong choice.
I think that it can be a really complicated set of feelings to come to terms with, when decisions were already made and you don’t know how they will affect your children growing up. What would you say to parents who want the best for their kids, and maybe did choose surgeries? How do we move forward in those conversations?
Stephani: Well, I think it’s important to have an honest conversation with your child about how you made choices with the information you had when you faced the decision. If you are feeling torn or conflicted or experiencing guilt, you can share that with your child. I’m human, too. I’ve made mistakes in my parenting. I was making the best choices that I could at the time, using the tools that I had.
So would I have made the same choice to delay surgeries for Wade if this was 25 years ago? I’m not ashamed to say: I probably would not have. I probably would have accepted the word of a physician, because I looked up to physicians. My family was part of the medical field for my entire life. I thought that they knew everything, that they were always going to speak to the best interest of every patient. Until it happened to me.
Talking about your guilt and talking about your feelings or why you made choices helps to heal everybody: yourself and your children. So it’s important to communicate and not keep secrets, because secrecy and privacy are different. If you’re feeling something, bring it up.
Hans: Yeah. That’s all any human person can do. We’re all human, we all want to do what’s best and we have to be able to talk about that.
Stephani: That’s why I feel like this is the real gift. Wade is a special kind of kid. I wouldn’t have traded any of my experiences for the world.
Hans: Well, he’s incredible, you’re incredible and I’m so grateful to you for this conversation and for all the incredible advocacy that you’ve been doing.
If you’re a parent going through this process, please reach out to interACT. We can connect you with Stephani and other parents. Also check out the Lohmans’ book, Raising Rosie, for more of the story.
This interview was edited for length and clarity and reviewed by interACT’s Medical Advisory Group.
Notes
- Lily C. Wang & Dix P. Poppas, Surgical Outcomes and Complications of Reconstructive Surgery in the Female Congenital Adrenal Hyperplasia Patient: What Every Endocrinologist Should Know, Journal of Steroid Biochemistry & Molecular Biology 2017 Jan;165 (Pt A):137-144 (“While all surgery is associated with potential postoperative infections, girls with CAH who have a common urogenital sinus are not predisposed to urinary tract infections (UTIs) prior to surgery. However, post-surgical complications such as vaginal stenosis may increase infectious complications in CAH girls as they get older.”); Zenia M. Nabhan et al., Urinary Tract Infections in Children with Congenital Adrenal Hyperplasia, Journal of Pediatric Endocrinology & Metabolism 2006 Jun;19(6): 815-820 (reporting UTIs in 8 out of 41 patients with CAH; 7 of the 8 had undergone feminizing genitoplasty, and all UTIs occurred after surgery; only one UTI was reported in a patient who had not undergone surgery).
- Estimates of how often individuals with Congenital Adrenal Hyperplasia who were raised as girls ultimately have a different gender identity range from a typically cited “low-end” estimate of about 5% (Arianne B. Dessens et al., Gender Dysphoria and Gender Change in Chromosomal Females with Congenital Adrenal Hyperplasia, Archives of Sexual Behavior 2005;34(4): 389-97) to higher rates from more recent studies, such as 12% (Vickie Pasterski et al., Increased Cross-Gender Identification Independent of Gender Role Behavior in Girls With Congenital Adrenal Hyperplasia: Results from a Standardized Assessment of 4- to 11-Year-Old Children, Archives of Sexual Behavior 2015;44: 1363-75) or 17% (Katinka Schweizer et al., Gender Experience and Satisfaction with Gender Allocation in Adults with Diverse Intersex Conditions (Divergences of Sex Development, DSD), Psychology & Sexuality 2013).