Traducción español: Laura Inter del artículo
Maddie Moran from interACT sits down with Dr. Casey Orozco-Poore, graduate of Harvard Medical School, for a conversation on their recent groundbreaking research on CAH and so-called “nerve-sparing” surgeries. Their research, done alongside Alex S. Keuroghlian, MD, MPH, is titled: Neurological Considerations for ‘‘Nerve-Sparing’’ Cosmetic Genital Surgeries Performed on Children with XX Chromosomes Diagnosed with 21-Hydroxylase Congenital Adrenal Hyperplasia and Clitoromegaly.
(Note: this interview contains discussion of medical and sexual abuse against children.)
Moran: First, can you share a little background with us? What is Congenital Adrenal Hyperplasia (CAH)?
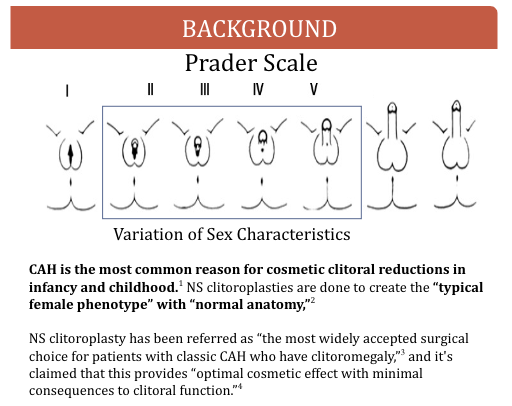
Dr. Orozco-Poore: CAH is associated with variations in sex development, particularly a larger than average clitoris at birth. The most common variant of CAH is one in which there is too little 21-hydroxylase, an enzyme that helps make cortisol. When that enzyme goes down, people may not be able to make enough cortisol. The enzyme deficiency also results in an increase in androgens. CAH exists in a spectrum, with some patients needing cortisol replacement therapy and others not. People with CAH can have increased androgens either at birth, or throughout development. Some aspects of CAH do need medical intervention such as cortisol replacement. However, cosmetic surgeries to “improve” the appearance of the clitoris are not medically necessary.
Moran: Why is it that cosmetic surgeries are happening on children with CAH?
Dr. Orozco-Poore: I use the word “cosmetic” in this paper, because the whole point of these surgeries is to improve the cosmesis of infant and young children’s genitalia from the perception of a surgeon.(1) This is different from gender-affirming surgeries for trans people, that center the decision-making of the individual.
These surgeries are happening because when babies with XX chromosomes are exposed to higher than average levels of androgens—so, testosterone—while they’re developing, they can be born with a larger than average clitoris. There’s nothing inherently wrong or concerning about that. Surgeons—predominately white, male, older surgeons—have decided that it’s not aesthetically pleasing for children to have larger than average clitorises and so they advocate for [portions of] the clitoris to be removed.
Modern medical literature discloses that the goal of medical care for CAH is to decrease the risk of “homosexuality”(2) and “gender identity disorder.”(3) That means the stated goal of these surgeries is to decrease the chances of someone being gay or bisexual, trans, or not identifying in a female role. It’s to increase the chances of having “successful” intercourse with a male husband, of being a “normal” female.
CAH is viewed as this kind of controversial area in intersex advocacy because doctors are saying, “people are happy with their early surgeries,” “people want early surgeries,” “people aren’t having sexual difficulties.” A big one is, “these surgeries are nerve-sparing! We’ve made such a significant advancement in clitoral reductions!” However, I’ve found these claims are not substantiated.
Moran: Tell us about “nerve-sparing” surgeries, and if this claim holds up?
Dr. Orozco-Poore: The Dix Poppas nerve-sparing surgery is frequently cited in the literature as being this pivotal event in care for CAH. So instead of doing a clitorectomy, or a clitoral reduction that removes the dorsal nerve, efforts are made to not intentionally remove the dorsal nerve. They do this by cutting the tissue and then removing the interior spongy tissue of the clitoris completely.
Just some basic anatomy—the dorsal nerve is considered part of the somatic nervous system. That’s the system that’s responsible for touch and sensation. They really tried to preserve the dorsal nerve trunk. However, by removing the entire spongy tissue within the clitoris, they’re removing the entire cavernous nerve—part of the autonomic nervous system. An example of cavernous nerve function is to engorge the clitoris during arousal.
They removed thousands and thousands of neurons, which could potentially be as much as a third of the neurons that are present in a clitoris.(4) They said those nerves are not important because they’re “just the branches of the dorsal nerve.”(5)
Hard stop. Just for basic neurology 101, the branches of larger nerves are what allow the larger nerves to receive signals. If you cut off the branches of the tree and you cut off all the leaves, the tree will not be able to receive signals from the sun through their leaves. The large nerve needs its branches, because with its branches it is able to connect with the body and understand what the body is feeling.
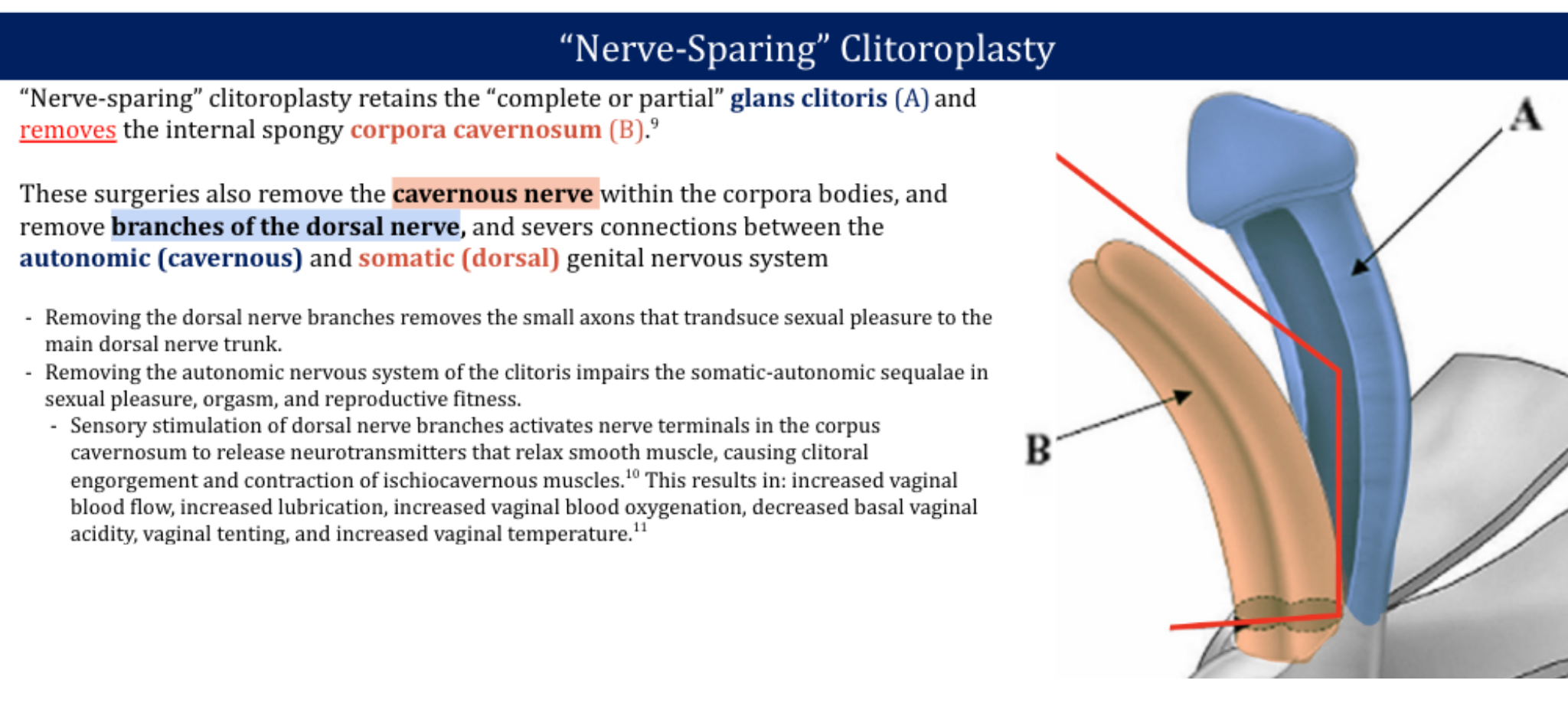
In the Dix Poppas study, they kept saying, “These nerves are insignificant because they’re small.”(6) They’re actually significant because they’re small, they’re the most important kind of nerve in the genitalia.(7) Removing them is unacceptable for sensation.
So they remove the dorsal nerve branches. They remove the connections between the cavernous nerve and the dorsal nerve—and there are connections between them.(8) They remove the entire cavernous nerve and all of the spongy erectile tissue of the clitoris leaving it down to a stump. That is neurologically devastating.
Moran: What are the risks of cutting these nerves for sexual sensation?
Dr. Orozco-Poore: The risk is that you don’t have the right to a fully functioning nervous system. The medical establishment is robbing the right of intersex people to have access to their intact neurological, sexual and reproductive outcomes.
We talk very little about how the clitoris actually has a reproductive role. Clitoral stimulation increases vaginal blood flow, lubrication, acidity, vaginal temperature, vaginal tenting.(9) Those are all really important things to ensure that someone is able to be at their peak fertility. By removing most of the clitoris you’re decreasing someone’s reproductive potential.
Right around the time that Dix Poppas was showing the scientific community the surgeries, in 2008 there was a study that evaluated newer nerve-sparing surgical techniques, and found that they had the worst possible score for difficulty orgasming. Every single patient who underwent clitoral reduction—all reported decreased sensation to warm, cold and vibration.(10)
Moran: For those who don’t know—can you talk more about Dix Poppas and why his research was so harmful?
Dr. Orozco-Poore: The way that Dix Poppas tried to prove his studies work were with extremely harmful post-surgical methods that intersex individuals have defined as sexual abuse and modern-day ethicists have condemned.(11)
Dix Poppas, in order to prove that his surgeries were nerve-sparing, applied a vibrator to the clitorises of young children with an average age of 5-7.(12) He applied a vibrator to the clitoris and then to the inner thigh, and asked them which they felt more. What that looks like is young children, 5 years old, unable to consent, who just had a very neurologically devastating surgery, having a vibrator applied to their clitoris in front of their family and in front of their doctor. Which is horrific.

It’s also not very good science. There is a collection of 13 intersex narratives compiled by Geogiann Davis in which the word “pain” appeared over 30 times.(13) In all of Dix Poppas’ research, on the nerve-sparing surgeries and on the outcome study, the word “pain” is never mentioned. Someone might have increased sensation of the clitoris because of nerve damage. And having an increased sensation compared to the inner thigh does not predict normal sexual function. It does not predict a capacity to orgasm. It does not predict full reproductive potential. It does not predict sexual behavior without trauma and without pain.
Looking through Dix Poppas’ work and the work of pediatric urologists in general, I am continually shocked at the low-quality evidence and the human rights violations that are taking place.
Moran: Is it accurate to say that the Dix Poppas studies have informed current modern practices?
Dr. Orozco-Poore: Yes, the Dix Poppas study has been fundamental in informing modern practices. For example, in legislative sessions, CAH is often used as a justification for continued non-medically necessary cosmetic surgeries in childhood. [Nerve-sparing surgeries are] frequently cited as this seminal event. And so often intersex adults are gaslit by the medical establishment when they talk about their narrative, because doctors keep saying well now the surgeries are better, they’ve improved. But it is never right to remove the functioning sex organs, genitalia, gonads, etc. of a child. If someone has functioning organs that are not currently cancerous [and do not] have a very high likelihood of becoming cancerous, that is a normal part of biodiversity.
Moran: What would you say to a doctor or surgeon who says we just need even better nerve-sparing genital surgeries to treat children with CAH?
Dr. Orozco-Poore: If you are performing a surgery which removes a part of the body, you will always remove the nerves inside that part of the body, and the connections between that part of the body and the rest of the body. There is no way to do a truly nerve-sparing surgery if you are amputating an organ.
There’s actually no medical risk of having a large clitoris. You know what the main “risk” is, of having a big clitoris and not having it operated on? The main risk is that pediatric urologists lose money. CAH with 21- hydroxylase deficiency in individuals with XX chromosomes is the most common reason(14) for clitoroplasty in childhood. It is a money-generator.
Places like Boston Children’s Hospital have actually banned all clitoroplasties and vaginoplasties at their sites.

Pidgeon Pagonis, co-founder of the Intersex Justice Project, at a protest in 2017. Photo by Sarah-Ji, Intersex Justice Project
Moran: What further research would you like to see on this topic?
Dr. Orozco-Poore: For one, I don’t think any more neurological testing should be done on young children to try to prove that these surgeries “work.” They only benefit the surgeons who are trying to justify continued surgeries, and I strongly believe that there is enough evidence at this point to stop all clitoroplasties completely.
The studies that have been done by pediatric urologists suffer from participant bias, which has been described by Dr. Baratz and Feder.(15) Within Davis’s series of 13 narratives, an individual said, “When I was in my twenties, my doctor came to my house to ask my parents to be involved in a follow-up study. My mom spoke for me that day when she said, ‘My daughter feels like what you’re doing to her is sexual abuse.’ My mother told me that he did nothing in response. He said nothing. He simply walked out of my door and never looked back.”(16)
Are those people included in the studies? No.
My ideal study is a federal-level review on every single patient with CAH who has stepped foot in Weill Cornell. [Note: Dix Poppas is a practicing pediatric urologist and professor at Weill Cornell]. I’d really like to know, what is the percentage of people who felt that this procedure was sexual abuse, or were traumatized by this experience? What is the percentage of people whose parents regret these surgeries? What age did people end up grappling with their intersex identity? What age do they think these surgeries should have happened? Ideally, this study would be done in partnership with intersex justice organizations, to help facilitate a feeling of safety and community for folks who may have medical trauma.
I want to get questions from a sample size that’s more like 100% and less like 30%. That would give us actually an accurate study as opposed to these pediatric urology studies that are pulling from the same patients that have a good relationship with their surgeon.
Moran: What do you hope people will take away from your research?
Dr. Orozco-Poore: I hope people take away that removing a part of the body will remove the nerves within it, and the fact that pediatric urologists are being intentionally deceptive about that should bring great pause, for one. I would like to tell parents of intersex kids, be cautious of pediatric urologists pushing surgery because they have a great financial stake in continuing to do these surgeries.
And really, these surgeries are conversion efforts. So often, intersex people are denied that language. We use [terms like] conversion efforts for trans and gay people but we don’t define intersex surgery as conversion efforts. I argue that they are just as harmful and just as violent as conversion efforts.

We need government protections of people with sex characteristic diversity.
I am very wary of government power, I am very wary of legislators weighing in on medical decisions. We’ve seen how that can go so wrong—in abortion, in trans care. But because of the severe, consistent and intentional human rights violations that pediatric urologists continue to carry out, it has become necessary to pursue legislative protections for intersex youth to ensure physicians respect the human rights of people with sex characteristic diversity.
This interview has been edited for length.






